Therapy and Support for Autism Spectrum Disorder
The 2023 Autism CRC Guidelines for ASD Therapy and Support
In 2023, Australia released significant updates to its national guidelines for supporting autistic children and their families, with a strong focus on treatment and intervention. The new guidelines, led by Autism CRC, represent the first national, evidence-based framework in Australia that specifically addresses therapy and intervention choices for autistic children.
Key features of the 2023 ASD treatment guidelines:
- Evidence-Based, Individualised Care: The updated guideline provides clinicians and families with a structured but flexible roadmap to set therapy goals, select appropriate treatments, and measure progress. The emphasis is on tailoring supports to the individual needs and preferences of the child and family, rather than recommending a single approach for all (UWA).
- Neurodiversity-Affirming Practice: The 2023 edition places greater focus on neurodiversity-affirming principles, supporting positive identity and inclusion, and moving away from deficit-based models (Autism CRC).
- Scope of Interventions: The guidelines cover a broad range of interventions, including behavioural, developmental, therapy-based, and family-centered approaches. They help families and practitioners understand what is evidence-based and how to critically assess therapy options (Autism CRC).
- Collaborative Goal-Setting: There is a strong emphasis on shared decision-making between clinicians, children, and families to ensure that chosen therapies align with the child’s strengths, interests, and family values (UWA).
- Practical Resources: The guidelines are designed to be user-friendly, including resources and tools for both practitioners and families, making it easier to navigate the therapy landscape (Autism CRC).
Interventions for ASD
-
Behavioral Interventions
- Includes approaches like Applied Behaviour Analysis (ABA), Positive Behaviour Support (PBS), and other structured behavioural programs,
- Focus: Teaching specific skills, reducing challenging behaviours, and supporting adaptive functioning.
- Implementation: Delivered by trained professionals (e.g., psychologists, behaviour therapists) and may involve intensive, goal-oriented sessions. Family members are often coached to reinforce strategies at home (Autism CRC, Raising Children Network).
-
Developmental Interventions
- These approaches, such as the Developmental, Indivi,dual-difference, Relationship-based model (DIR/Floortime), Early Start Denver Model (ESDM), and Pivotal Response Therapy focus on promoting social interaction, communication, and emotional development.
- Implementation: Provided by allied health professionals (speech therapists, occupational therapists, psychologists), often in natural settings (home, childcare, community). Parents are key partners in delivering intervention through everyday activities
-
Therapy-Based Interventions
- Speech therapy, occupational therapy, and physiotherapy are commonly used to target communication, sensory processing, motor skills, and daily living activities.
- Implementation: Individual or group sessions led by registered therapists; goals are set collaboratively with families based on the child’s unique needs and strengths.
-
Family and Parent-Mediated Interventions
- Interventions that train and empower parents/caregivers to support their child’s development and behaviour at home.
- Implementation: Delivered through workshops, coaching, and ongoing support. Emphasis is on building parent confidence and skills, as well as supporting family wellbeing.
-
Education and School-Based Supports
- Encompasses individualised learning plans, adjustments to classroom environments, teacher training, and inclusion supports.
- Implementation: Collaborative planning between families, educators, and allied health professionals; supports are tailored to the child’s needs and regularly reviewed.
-
Psychological and Mental Health Interventions
- Includes cognitive-behavioral therapy (CBT) for anxiety or emotional regulation, as well as counselling and mental health support.
- Implementation: Delivered by psychologists or mental health professionals, often adapted for communication style and cognitive level of the child .
-
Medical and Pharmacological Interventions
- Used only when necessary for co-occurring conditions (e.g., ADHD, anxiety, sleep problems).
- Implementation: Prescribed and monitored by paediatricians or psychiatrists, always as part of a broader support plan
How Interventions Are Implemented in Practice
- Individualisation: All interventions are tailored to the child’s strengths, needs, and family context. There’s no “one-size-fits-all;” clinicians work with families to select and adapt interventions.
- Collaborative Goal-Setting: Families, children (where possible), and professionals jointly set therapy goals and regularly review progress.
- Evidence-Based Decision-Making: The guidelines provide tools for families and clinicians to evaluate the evidence behind therapies, ensuring choices are informed by quality research.
- Neurodiversity-Affirming: Interventions aim to support skills, participation, and wellbeing, not to “normalise” autistic traits.
- Ongoing Review: Interventions are monitored, and goals are adjusted as the child’s needs and circumstances change.
Attention deficits in ASD
One of the most common behaviour of children with Autism, is their lack of focus, joint attention, concentration and compliance. These attention deficits are usually treated with stimulant medication and help many children with ASD concentrate. When parents object to medication, and for those who do not respond well may benefit from Neurofeedback. Neurofeedback has been extensively researched since 1970 and found to be somewhat effective for ADHD children who have similar issues. The Australian clinical guidelines for ADHD do not recommend neurofeedback as stand alone or first line treatment for ADHD. However when medication is not suitable or not wanted by parents, Neurofeedback can be used as part of a multimodal program that include cognitive, behavioural strategies, parental education, dietary and lifestyle recommendations.
QEEG-guided Neurofeedback therapy for ADHD in children with Autism

In the Biomedical abnormalities in Autism Spectrum Disorder page on this website we outline a few of the many neurological abnormalities that have been found in children with ASD. Remember that every child has a unique subset of these abnormalities. Neurological abnormalities are reflected as abnormalities in the "brain's electrical activity", which in turn drive the behaviours observed in children with Autism. QEEG is a non-invasive tool to statistically compare the brainwaves of an individual to those brainwaves stored in a database of typically developing/functioning people of the same age (age range: 3 to 79 years).
The statistical differences are then represented in coloured maps, often called Brain maps. Note that this process is very different to the conventional EEG examination performed by a Neurologist, who visually examines the electrical brainwaves for "epileptiform", a pattern of complex waves suggestive of epilepsy.
Brain electrical activity is divided into bands of individual frequencies called Hertz (Hz for short). Although all brainwave frequencies are present in the EEG, it is the excesses or deficits at specific locations that are associated with abnormal behaviours.
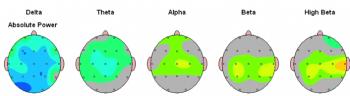
Delta waves (1-4 Hz) are normally seen predominantly in infants and in deep sleep. Excesses in delta suggest low blood flow and significant brain dysfunction, lethargy, drowsiness, and/or cognitive impairment. Deficits suggest sub-optimal serotonin neuromodulation, and is one of the patterns associated with flat mood and depression.
Theta waves (4-8 Hz) are normally seen in young children. Excesses in theta are associated with reduced blood flow and is frequently seen in children and adults with attention deficits disorder and learning difficulties.
Alpha waves (8-13 Hz) are normally produced in the resting state of the brain. They are normally associated with relaxation, meditation and self-awareness. Excessive alpha can be a sign of learning difficulties, attention deficits, emotional instability and/or depression.
Beta waves (13-21 Hz) and High Beta(21-30 Hz) waves Are normally associated with alertness and information processing. Excess beta waves at frontal sites is associated with anxiety, excitability, hyper-vigilance, irritability and poor sensory integration. Global excesses may be from environmental toxins which cause cortical irritability and scramble information processing. Deficits suggest a lack of electrical power and are associated with reduced information processing capacity.
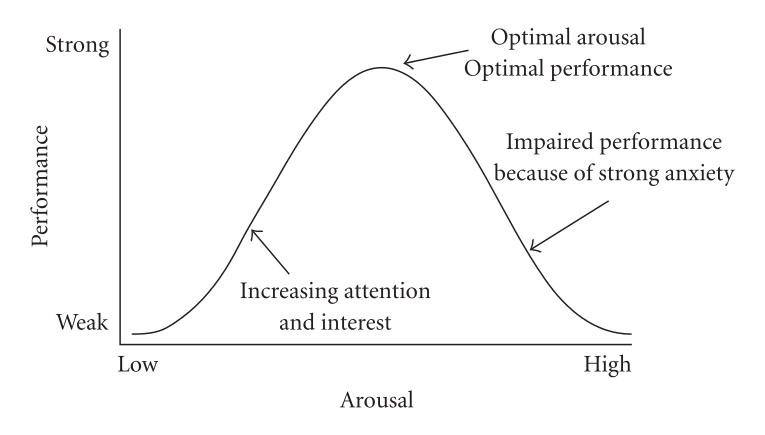
The graph on the left represents how for each frequency there is an optimum power level for optimum performance. Although, as a group, there are common denominators in the brainwaves and behaviours of children with Autism, there are also many individual differences.
Hence, Neuroscientists and clinicians do not look for patterns in the brain maps that will identify Autism, as there is no such single pattern. Instead, we look for statistically recognisable features that have been associated with specific behaviours. There are thousands of studies that have associated excesses or deficits in brainwaves at specific locations, with various behavioural manifestations, such as: attention deficits, learning difficulties, receptive or expressive language deficits, depressed mood, anxiety, OCD, ODD and other behavioural differences.
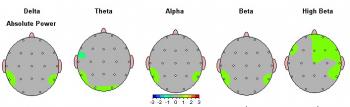
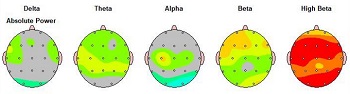
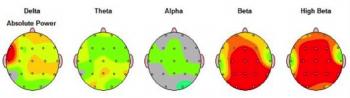
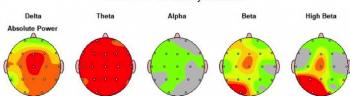
The Brain maps below represent brain electrical activity as "differences from normal". Grey and one colour on either side of grey on the scale are in the normal range. The cooler blue colours progressively indicate deficits, while the warmer red colours progressively indicate excesses. To keep things simple, we are only looking at differences in power levels in frequency bands here. In research and clinical practice, we also look at differences in individual frequencies and coherence (connectivity) between different areas of the brain, and asymmetries, left to right and back to front. All of which gives us information about brain "function". The first brain map below is that of a typically developing child with no disorders and the next four brain maps (Cases 1-4) demonstrate how different the brain of children with ASD can be.
QEEG and ASD Research
Here are links to a few of the many studies studies regarding QEEG in Autism Spectrum disorder:
- BRAIN CONNECTIVITY IN AUTISM. This publication, from Frontier in Human Neuroscience, contains a series of 15 separate studies on QEEG in Autism Spectrum Disorder
- QEEG characteristics and spectrum weighted frequency for children diagnosed as autistic spectrum disorder
- EEG power and coherence in autistic spectrum disorder.
- On the Application of Quantitative EEG for Characterizing Autistic Brain: A Systematic Review.
- Autism and EEG phase reset: deficient GABA mediated inhibition in thalamo-cortical circuits.
- Resting state EEG abnormalities in autism spectrum disorders
- QEEG-guided neurofeedback
- Brainmaps highlight Autism Disorders
- QEEG-Guided Neurofeedback for Autism: Clinical Observations and Outcomes
- A review of the use of EEG connectivity to measure the neurological characteristics of the sensory features in young people with autism
- Is functional brain connectivity atypical in autism? A systematic review of EEG and MEG studies
- Name recognition in autism: EEG evidence of altered patterns of brain activity and connectivity
- Toward an Interdisciplinary Understanding of Sensory Dysfunction in Autism Spectrum Disorder: An Integration of the Neural and Symptom Literatures
- Neural Correlates of Sensory Hyporesponsiveness in Toddlers at High Risk for Autism Spectrum Disorder
- EEG Coherence Patterns in Autism: An Updated Review
- Standard Electroencephalography in Clinical Psychiatry: A Practical Handbook
- Brain Connectivity in Autism Spectrum Disorder
- A review of the use of EEG connectivity to measure the neurological characteristics of the sensory features in young people with autism
Neurotherapy for attention deficits in ASD

Neurotherapy is based on the principles of learning theory, ABA therapy and operant conditioning. Namely, when we reward a behaviour, we increase the likelihood of that behaviour being repeated. During a Neurotherapy session, the person has a sensor placed at a specific location where we want to improve function. this sensor is connected to an electroencephalographic device which sends the Brain's electrical activity at that location to a computer software. The software extracts the specific frequencies that we want to reward and/or suppress and displays them as levels on bar charts on the left of the screen. Typically, reward criteria is met when the slow waves are below its set threshold and the fast waves above its set threshold.
When the reward criteria are met the child is rewarded for producing the brainwave pattern that we want to promote. This increases the likelihood of the appropriate brainwaves being produced more frequently. The visual and auditory reward feedback may be in the form of a video which will play at full intensity and normal sound level or PACMAN will move, or "Space invader game" will allow firing of lasers.
Here are links to a few of the many studies studies regarding Neurotherapy in Autism Spectrum disorder:
- Baruth, J., Casanova, M., El-Baz, A., Horrell, T., Mathai, G., Sears, L., Sokhadze, E. (2010). Low-frequency repetitive transcranial magnetic stimulation modulates evoked gamma frequency oscillations in autism spectrum disorder. Journal of Neurotherapy, 14(3), 179–194.
- Coben, R. Middlebrooks, M., Lightstone, H. and Corbell, M. (2018) Four Channel Multivariate Coherence Training: Development and Evidence in Support of a New Form of Neurofeedback. Front. Neuroscience 12: 729. PMID: 30364276
- Coben, R., Mohammad-Rezazadeh, I., Cannon, R. (2014). Using quantitative and analytic EEG methods in the understanding of connectivity in autism spectrum disorders: a theory of mixed over- and under-connectivity. Frontiers in Human Neuroscience 8:45. doi: 10.3389/fnhum.2014.00045.
- Coben, R., & Myers, T. E. (2010). The relative efficacy of connectivity guided and symptom based EEG biofeedback for autistic disorders. Applied Psychophysiology & Biofeedback, 35(1), 13–23.
- Coben, R., & Pudolsky, I. (2007). Assessment-guided neurofeedback for autistic spectrum disorder. Journal of Neurotherapy, 11(1), 5–23.
- Coben, R., (2007). Connectivity-guided neurofeedback for autistic spectrum disorder. Biofeedback, 35(4), 131–135.
- Coben, R., Sherlin, L., Hudspeth, W. J., McKeon, K., & Ricca, R. (2014) Connectivity-Guided EEG Biofeedback for Autism Spectrum Disorder: Evidence of Neurophysiological Changes. Journal of NeuroRegulation, 1(2) 109-130.
- Drysdale, M,T,B., Martinez, Y, J., Thompson, L. (2012). The effects of humorous literature on emotion: A pilot project comparing children with asperger’s syndrome before and after neurofeedback training and controls. Journal of Neurofeedback.
- Friedrich, E., Sivanathan, A., Lim, T., Suttie, N., Louchart, S., Pillen, S., Pineda, J. (2015). An effective neurofeedback intervention to improve social interactions in children with autism spectrum disorder. Journal of Autism & Developmental Disorders, 45(12), 4084-4100. doi: 10.1007/s10803-015-2523-5
- Frye, R., Rossignol, D., Casanova, M., Martin, V., Brown, G., Edelson, S., Coben, R., Lewine, J., Slattery, J., Lau, C., Hardy, P., Fatemi, S., Folsom, T., MacFabe, D., Adams, J. (2013). A review of traditional and novel treatments for seizures in autism spectrum disorder. Findings from a systematic review and expert panel. Public Health 1:31. doi: 10.3389/fpubh.00031
- Goodman, M. S., Castro, N., Sloan, M., Sharma, R., Widdowson, M., Herrera, E., Pineda, J. A. (2018). A Neurovisceral Approach to Autism: Targeting Self-Regulation and Core Symptoms Using Neurofeedback and Biofeedback. NeuroRegulation 5(1), 9-29.
- J. R. Evans (Ed.), Handbook of Neurofeedback. Binghampton, NY: Haworth Medical Press. "The whole Book"
- Jarusiewicz, G. (2007). Use of neurofeedback with autistic spectrum disorders. Chapter in J. R. Evans (Ed.), Handbook of Neurofeedback. Binghampton, NY: Haworth Medical Press, pp. 321–339.
- Jarusiewicz, B. (2002). Efficacy of neurofeedback for children in the autistic spectrum: A pilot study. Journal of Neurotherapy, 6(4), 39–49.
- Knezevic, B., Thompson, L., & Thompson, M. (2010). Pilot project to ascertain the utility of Tower of London Test to assess outcomes of neurofeedback in clients with Asperger’s Syndrome. Journal of Neurotherapy, 14(3), 3–19.
- Kouijzer , ME UJ., de Moor, JMH, Gerrits, BJL, Buitelaar, JK, & van Schie, HT (2009). Long-term effects of neurofeedback treatment in autism. Research in Autism Spectrum Disorders, 3(2), 496–501.
- Pineda J. A., Brang D, Hecht E, Edwards L, Carey S, Bacon M, Futagaki C, Suk D, Tom J, Birnbaum C, Rork A.(2008). Positive behavioral and electrophysiological changes following neurofeedback training in children with autism. Research in Autism Spectrum Disorders, 2, 557–581.
- Scolnick, B. (2005). Effects of electroencephalogram biofeedback with Asperger’s syndrome. International Journal of Rehabilitation Research, 28(2), 159–163.
- Sichel, A. G., Fehmi, L. G., & Goldstein, D. M. (1995). Positive outcome with neurofeedback treatment of a case of mild autism. Journal of Neurotherapy, 1(1), 6064.
- Sokhadze, E., Baruth, J., El-Baz, A., Horrell, T., Sokhadze, G., Carroll, T., Tasman, A., Sears, L., Casanova, M. (2010). Impaired error monitoring and correction function in Autism. Journal of Neurotherapy, 14(2), 79–95.
- Sokhadze, E. M., Casanova, M. F., El-Baz, A. S., Farag, H. E., Li, X. & Wang, Y. (2016). TMS-based Neuromodulation of Evoked and Induced Gamma Oscillations and Event-related Potentials in Children with Autism. NeuroRegulation, 3.(3), 101-126.
- Sokhadze, Guela & Casanova, Manuel & Kelly, Desmond & Casanova, Emily & Russell, Brook & Sokhadze, Tato. (2017). Neuromodulation Based on rTMS Affects Behavioral Measures and Autonomic Nervous System Activity in Children with Autism. NeuroRegulation. 4. 65-78. 10.15540/nr.4.2.65.
- Sokhadze, E., El-Baz, A., Tasman, A., Sears, L., Wang, Y., Lamina, E., Casanova, M. (2014). Neuromodulation integrating rTMS and neurofeedback for the treatment of autism spectrum disorder: an exploratory study. Applied Psychophysiology & Biofeedback, 39(3-4), 237-257. doi: 10.1007/s10484-014-9264-7
- Steiner, N., Frenette, E., Hynes, C., Pisarik, E., Tomasetti, K., Perrin, E., Rene, K. (2014). A pilot feasibility study of neurofeedback for children with autism. Applied Psychophysiology & Biofeedback, 39(2), 99-107. doi: 10.1007/s10484-014-9241-1
- Wang, Y., Sokhadze, E. M., El-Baz, A. S., Li, X., Sears, L., Casanova, M. F., Tasman, A. (2015). Relative power of specific EEG bands and their ratios during neurofeedback training in children with Autism Spectrum Disorder. Frontiers in Human Neuroscience, 9, 723.
- FOR A FULL NEUROTHERAPY BIBLIOGRAPHY LOOK UP THE ISNR WEBSITE




