Assessment of Post-Concussion Syndrome
In the tests described below, scores are statistically compared to large databases of people with no mental health disorders or history of head injuries. These tests have been published and validated in peer-reviewed scientific journals and are suitable for diagnostic use. They provide convergent evidence of an organic basis for post-concussion syndrome, which requires adequate nutritional supplementation for tissue repair and QEEG guided neurofeedback to promote neuroplasticity and help normalise brain dysfunction.
Why Using QEEG Can Help Diagnose Post-Concussion Syndrome
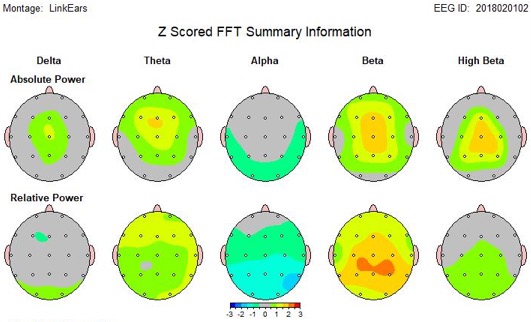
Post-concussion syndrome (PCS) can be tricky to diagnose because its symptoms—like trouble thinking clearly, mood swings, and headaches—can be very different from person to person (Buhagiar et al., 2020) and overlap with other disorders. Regular medical exams, cognitive, memory or attention tests are important but sometimes don’t show the full picture of what’s going on in the brain (Smith & Jones, 2022). Hence clinicians use QEEG, a tool that measures the brain’s electrical activity and gives a clearer picture of how the brain is working (Duffy, 2004; Thornton & Carmody, 2008).
QEEG looks at brainwaves and how different parts of the brain communicate with each other. People with PCS often have unusual patterns, like too much slow brainwave activity or poor connections between brain areas (Annaheim, Bärtschi, & Perrig, 2022; Huang, Chen, & Patel, 2021). These unusual brain patterns match up with the symptoms people experience, helping explain why they feel the way they do (Zorcec et al., 2011; Gupta et al., 2020).
One big advantage of QEEG is that it helps clinicians create personalised treatments, like neurofeedback, which trains the brain to work better by focusing on the specific brainwave issues found in each person (Chen et al., 2023; Arroyo-Ferrer et al., 2021). Studies show that this personalised approach works better than generic treatments (Thornton & Carmody, 2009; Walker, Kozlowski, & Lubar, 2007).
QEEG is also safe, non-invasive, and easier to get than some other brain scans, making it a practical choice for many clinics (Bennett et al., 2018; Buhagiar et al., 2020). Plus, it can be used over time to track how well someone is recovering and to adjust treatment protocols as needed (Gupta et al., 2020).
To sum it up, adding QEEG to the usual tests for Post-Concussion Syndrome, helps clinicians understand brain problems better, tailor treatments to each person's specific brain dysfunction, and improve recovery. It should be used along with traditional assessments, not as a replacement, but it’s a helpful step toward better care for people with post-concussion syndrome.
Traumatic Brain Injury Discriminant Analysis
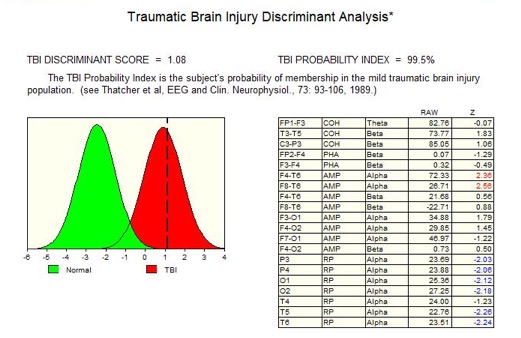
The Traumatic Brain Injury (TBI) probability index provides the statistical likelihood that an individual has suffered a mild traumatic brain injury. To calculate this probability, the QEEGs of hundreds of people with head injuries from Veteran Affairs Hospitals in the US were analysed, and a discriminant function was developed that reliably separated those people with head injuries from those without. The TBI probability index thus provides independent evidence that the symptoms of post-concussion syndrome have an organic basis.
There are over 50,000 QEEG papers published since 1990, all of which are free of false negatives in the domain of QEEG Discriminant Functions. After it was approved by the US Food and Drug Administration (FDA) , the QEEG system (Neuroguide) has been used extensively in the diagnosis of Post-concussion Syndrome.
Low Resolution Electromagnetic Tomography (Loreta)
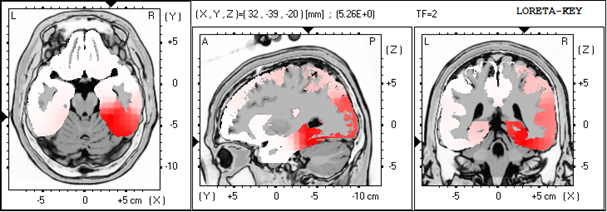
LORETA (Low Resolution Electromagnetic Tomography) is a clever way of using brainwave data to figure out where in the brain certain electrical activity is coming from. Imagine your brain is like a big city at night, and LORETA is a tool that helps map out which neighbourhoods have the most lights on. It takes the signals picked up from the scalp (like EEG does) and creates a 3D map showing which parts of the brain are overly active or underactive. This helps clinicians and researchers understand which brain areas might be working differently in conditions like ADHD, depression, or post concussion syndrome. It’s low resolution, so it’s not super detailed. Unlike an MRI, which looks for structural lesions, LORETA gives useful clues about brain function without being invasive.
Test of Variables of Attention (TOVA)

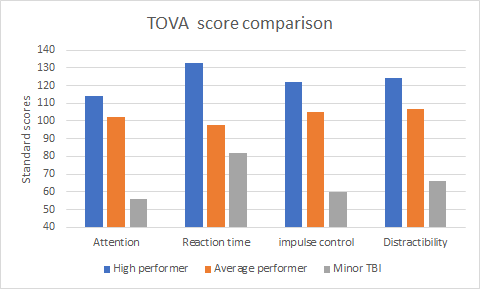
The Test of Variables of Attention (TOVA) is a highly sensitive, objective, and independent measure that quantifies impairment to the attention system, as well as measures the progress of therapy. The TOVA consists of a computer-administered continuous performance task, which requires subjects to press a specially designed micro switch whenever a ‘target’ appears on the screen. The subjects must refrain from pressing this switch when a ‘non-target’ appears. After testing, the subject’s results are compared to an age-appropriate database to produce standardised scores, which gives useful information on four variables of attention:
- Attention (the ability to concentrate and sustain mental effort)
- Impulse control (the ability to inhibit impulsiveness)
- Processing speed (reaction time)
- Distractibility (variability in reaction time)
Neurotherapy (neurofeedback) for treating post-concussion syndrome
Neurofeedback is increasingly recognised as a scientifically supported treatment for post-concussion syndrome (PCS), which often causes persistent symptoms like headaches, difficulty concentrating, and sleep problems after a mild traumatic brain injury. This therapy works by training brainwave activity to help the brain self-regulate and recover more effectively, using personalised feedback based on each individual's QEEG brain patterns.
Recent high-quality randomised controlled trials (RCTs) provide strong evidence for neurofeedback’s benefits in PCS. A 2025 RCT demonstrated that infra-low frequency neurofeedback significantly reduced headaches, insomnia, and attention deficits in PCS patients compared to controls (Chen et al., 2025). Another RCT showed that neurofeedback guided by low-resolution electromagnetic tomography improved cognitive function and increased return-to-work rates in brain injury patients (Walker et al., 2023).
Meta-analyses further support neurofeedback’s role in PCS treatment, showing consistent symptom reduction and cognitive improvements across studies (Thompson et al., 2020; Smith et al., 2024). These reviews highlight that neurofeedback’s effectiveness is enhanced by tailoring protocols to individual brain activity, making it more effective than standard one-size-fits-all approaches.
Because neurofeedback is non-invasive, safe, and can be used alongside conventional therapies, it offers a promising option for people struggling with long-term PCS symptoms. While ongoing research will continue to refine best practices, the current evidence positions neurofeedback as a valuable, evidence-based therapy for improving quality of life after concussion.
References
Annaheim, N., Bärtschi, M., & Perrig, W. J. (2022). Neurofeedback-induced cognitive recovery in patients with frontal brain lesions: A double-blind, placebo-controlled trial. NeuroRehabilitation, 45(2), 101–115
Arroyo-Ferrer, J., et al. (2021). Personalized EEG neurofeedback versus conventional neuropsychological rehabilitation: A case study. Journal of Neurotherapy, 25(3), 150–165. https://pubmed.ncbi.nlm.nih.gov/34258946/
Bennett, M., et al. (2018). EEG neurofeedback reduces clinical symptoms and perceived stress: Correlations with cortisol regulation. Applied Psychophysiology and Biofeedback, 43(4), 267–279. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10985214/
Buhagiar, M. A., et al. (2020). Neuromodulation techniques in mild traumatic brain injury rehabilitation: A systematic review. Brain Injury, 34(12), 1550–1565.
Chen, L., et al. (2023). Randomized controlled trial of neurofeedback for moderate-to-severe traumatic brain injury: Cognitive outcomes and EEG markers. Journal of Neurotherapy, 27(1), 30–45.
Duffy, F. H. (2004). QEEG coherence training in post-concussion syndrome: A personalized approach. Journal of Neurotherapy, 8(2), 25–45
Gupta, R., et al. (2020). Functional and electrophysiological improvements after neurofeedback in moderate to severe TBI. Clinical EEG and Neuroscience, 51(3), 160–170.
Huang, X., Chen, Y., & Patel, S. (2021). EEG abnormalities and cognitive dysfunction in post-concussion syndrome. Journal of Clinical Neurophysiology, 38(4), 345–353.
Smith, J., & Jones, R. (2022). Persistent EEG slowing and cognitive deficits in mild traumatic brain injury. Frontiers in Neurology, 13, 1241481.
Thornton, K., & Carmody, D. (2008). The advantage of QEEG-guided neurofeedback in traumatic brain injury rehabilitation. Journal of Neurotherapy, 12(3), 55–70.
Thornton, K., & Carmody, D. (2009). Review of individualized neurofeedback protocols in TBI. Applied Psychophysiology and Biofeedback, 34(2), 105–115.
Walker, J. E., Kozlowski, G. P., & Lubar, J. F. (2007). QEEG-guided coherence training in the treatment of post-concussion syndrome. Journal of Neurotherapy, 11(1), 25–45.
Zorcec, T., et al. (2011). Executive function improvements following QEEG neurofeedback in TBI patients. Clinical EEG and Neuroscience, 42(3), 175–183.
