ADHD Test, Symptoms & Causes
ADHD can manifest with or without hyperactivity . Most children with ADHD can be well behaved and polite and are beautiful children of normal intelligence and many have above average intelligence. However, they can often be overly inattentive and be easily distracted, they can be fidgety and may tend to make impulsive mistakes and some can be hyperactive.
In the media, ADHD is often mischaracterised as being solely associated with hyperactivity, but this is not representative of the ADHD community. Due to this, parents with the inattentive subtype of ADHD are often reluctant to accept that their child, who has no hyperactivity or behavioural challenges, meets diagnostic criteria.
Diagnosis and treatment of ADHD
In accordance with the Diagnostic and Statistical Manual of Mental Disorders (DSM-V), ADHD is first diagnosed through gaining a clinical history before the parent and/or child fills out behavioural questionnaires. The DSM-V, in all its iterations, was designed by the American Psychiatric Association to help prescribe psychiatric medication.
ADHD Treatment According to Clinical Guidelines
The 2022 Australian ADHD Professionals Association (AADPA) clinical guidelines provide an evidence-based framework for the diagnosis and management of ADHD in children and adolescents. The guidelines emphasise a multimodal treatment approach tailored to individual needs, combining pharmacological and non-pharmalogical interventions.
Pharmacological Treatment:
Stimulant medications, including methylphenidate and dexamphetamine, are recommended as first-line pharmacotherapy due to their strong evidence of efficacy and safety in reducing core ADHD symptoms. Medication should be carefully titrated and monitored, considering potential side effects and coexisting conditions such as anxiety (AADPA, 2022).
Psychosocial Interventions:
Behavioural therapies, particularly cognitive-behavioural therapy (CBT), parent training, and school-based support, are essential components of comprehensive ADHD management. These interventions address emotional regulation, oppositional behaviours, and functional impairments, complementing medication effects (AADPA, 2022).
Neurofeedback:
While neurofeedback shows some promise as an adjunctive therapy, the AADPA guidelines do not endorse it as a first-line treatment. The guidelines state that neurofeedback is an emerging treatment for core symptoms. However, the current evidence is limited by methodological variability and inconsistent outcomes and more research is needed before it can be recommended as first line treatment. However, after discussing potential benefits and limitations. neurofeedback may be considered for families seeking non-pharmacological options or when medication is contraindicated or poorly tolerated, Neurofeedback should be integrated within a broader multimodal plan and delivered by experienced clinicians with ongoing outcome evaluation (AADPA, 2022).
Lifestyle and Nutritional Considerations:
The guidelines highlight the role of lifestyle factors, recommending regular physical activity, sleep hygiene, and nutritional assessment to support symptom management and overall well-being. Dietary interventions should focus on balanced nutrition and correction of deficiencies but are adjunctive rather than primary treatments (AADPA, 2022).
ADHD Assessment in Adults & Children
According to the DSM-5, a diagnosis of ADHD applies to children and adults who consistently display certain behaviours over time.
Traditionally, ADHD is diagnosed if the child meets a characteristic behaviour. So broad is the list of behaviours in the DSM-V that it captures nearly all childhood problems. Children with attentional disorders range from polite, dreamy, and inattentive to hyperactive.
Science has yet to identify ‘the cause’ behind these different presentations, and it remains unlikely that a single cause for ADHD will ever be found. Over the years, several causal factors have been proposed. The wide range of symptoms present in ADHD suggest that ADHD is better characterised as a term which captures many underlying disorders. If ADHD constitutes many disorders, then it makes sense that there are such diverse behavioural manifestations and not all respond to stimulant medications.
Quantitative electroencephalography (QEEG).
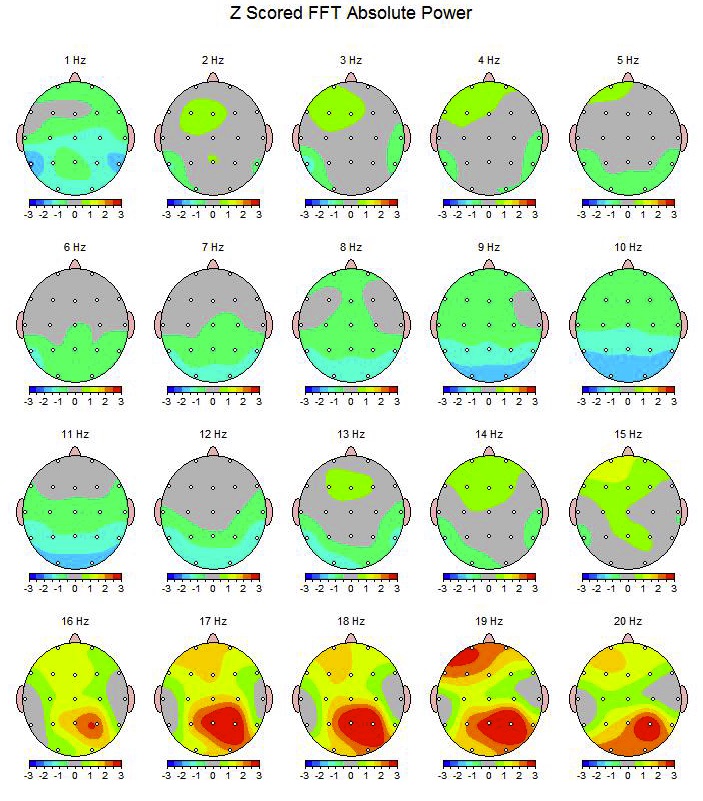
Quantitative EEG (QEEG) is the statistical analysis of the electrical activity of the brain. It is a brain mapping tool used to evaluate differences in brain function compared to a database of people without difficulties. In the brain map image, the colour grey, and one colour gradation above and below on the scale, represent the normal range.
The hotter colours represent excesses of brain electrical activity and colder colours represent deficits. Some of these excesses and deficits are related to specific behavioural and learning difficulties, or mood disorders. QEEG enables the formulation of therapy options guided by these brain patterns, rather than simply relying on behavioural questionnaires.
QEEG is useful in revealing the underlying abnormal brainwave patterns associated with ADHD and other disorders. QEEG can help clinicians discriminate between ADHD that are likely to respond to stimulant meds and neurofeedback from those who may not.
Test of Variables of Attention (T.O.V.A)
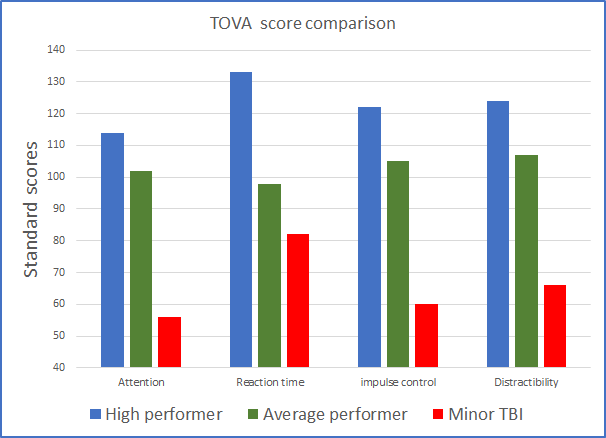
The TOVA is a computer administered continuous performance test which is widely used as a screening tool for ADHD. It is not a diagnostic tool. The TOVA is an objective method for assessing the effectiveness of medication for ADHD, without relying solely on parental/teacher reports and interviews.
BNC offers the TOVA as a service for paediatricians to titrate prescription ADHD medication. Parents can ask their paediatrician for this test to be administered before medication is prescribed, so that the dosage is adjusted appropriately.
The TOVA reduces the likelihood of under or over-medication. It ensures that the medication is optimum for the child. A computer-generated report is provided to the referring medical practitioner (or to the parents).
The TOVA scores below compare a child with ADHD who has a minor head injury (mTBI), caused by a fall off a bicycle, to an average or high performer on the test.
The TOVA requires clients to press a micro switch whenever a ‘target’ appears on the screen, and to refrain from pressing it when a ‘non-target’ appears. The scores are compared to age-appropriate norms, which gives us useful objective information on four variables of attention:
-
Ability to sustain attention and mental effort.
-
Impulse control.
-
Brain processing speed (reaction time).
-
Distractibility (variability in the response times).
Wechsler Intelligence Scale for Children (WISC V)
The WISC V tests general thinking and reasoning skills of students aged 6-16. The scores show how well a student compares to thousands of students, of the same age, from across the US and Australia. The highest possible score is 160, and the lowest possible score is 40. Half of all students will score less than 100, and half of all students will score more than 100. Scores from 90 to 109 are considered average. This test has three main scores: a Verbal IQ score, a Performance IQ score, and a Full-Scale IQ score. The Verbal IQ score indicates how well a student does on tasks that require listening to questions and giving spoken answers.
These tasks evaluate the skills required for understanding verbal information, thinking with words, and expressing thoughts in words. The Performance IQ score indicates how well a student does on tasks that require examining and thinking about design, pictures, puzzles and solving problems without using words. The tasks evaluate skills in solving non-verbal problems using hand-eye coordination and working quickly and efficiently with visual information. These skills are often referred to as visuospatial skills.
The Verbal and Performance scores are combined into the Full-Scale IQ score. The WISC-V Full-Scale score is a way to view a student's overall thinking and reasoning skills.
The WISC-V has 13 subscales which are used to assess various aspects of verbal and non-verbal (visuo-spatial) intellectual skills. The results give a good indication of which cognitive functions are lacking before a therapy plan is formed.
Tests from Nutritionist or Dietician
Red Cell Essential Fatty Acid Profile
Every cell in the body has a lipid membrane protecting its boundaries. The brain consists of 70% lipid and 40% of the brain is made up of the long chain Omega 3 EFAs (of the kind we get from fish). Studies consistently indicate that deficiencies of Omega 3 EFAs are associated with serious brain and systemic dysfunctions. Research demonstrates that Omega 3 EFAs are essential for brain function, and deficits in them are associated with psychological disorders such as ADHD and ASD. The red cell Essential Fatty Acid Profile blood test reveals the composition of red cell fatty acids and identifies specific EFA deficiencies.
Omega 3 EFAs and Gut function
The gut cell wall (epithelium) is exposed to billions of organisms and toxins daily. The lipid membrane of each cell in the epithelium serves as a vital protective barrier. If the lipid membrane lacks Omega 3 fatty acids, protection fails and unfriendly organisms, irritants, and toxins, irritate the gut wall and can give rise to symptoms of IBS and Inflammatory Bowel Diseases. There are several other nutrients and systems involved that need to be considered.
Extended Faecal Microbiology Analysis (FMA)
Intestinal dysbiosis is a term used to describe an imbalance in the gut commensal (normally resident) microbiome. When the balance of the gut bacteria is thrown off, usually due to a diet high in sugars and refined carbohydrates, the gut contents become more acidic. This promotes the overgrowth of Streptococcus and undergrowth of e-Coli. Bioscreen Medical, has reported gastrointestinal changes in the abnormal faecal tests of patients with IBS, as well as those with ASD and anxiety. These observations have enabled our dietician and nutritionist to formulate effective therapy protocols, which have resulted in significant improvements in gut function in IBS sufferers.
This Bioscreen test, from a NATA accredited laboratory, is used to determine the profile of gut commensals (normal communities of bacteria). It is the only commercially available test in the world that accurately estimates the populations of commensal bacteria. The process involves keeping the faecal sample refrigerated in an anaerobic pouch to ensure that no oxygen reaches the sample prior to its analysis. If this does not happen, anaerobic bacteria would die upon air exposure during transportation, whilst the aerobes would continue to reproduce. Therefore, the Bioscreen method is highly accurate. The bacteria are grown over 3 weeks and counted to estimate the bowel’s profile. This test is not the same as parasitology and pathogen tests which are used to look for pathogenic bacteria and parasites.
Subtypes & Symptoms of ADHD
According to the DSM-V, there are three subtypes of ADHD which will be discussed below:
1. ADHD, Predominantly Inattentive Subtype.
This subtype takes into consideration the person’s age and is diagnosed if symptoms of inattention have persisted for at least 6 months. A child with inattentive ADHD may not pay attention to details or make careless mistakes. This child may have difficulty sustaining attention in tasks and play and may listen when spoken to directly. Often this child does not follow requests, complete schoolwork, and chores. They may have organisational difficulties or be forgetful – losing necessary things like pencils and books. They may be reluctant to engage in tasks that require sustained mental effort. Family life could be filled with arguments about homework.
2. ADHD, Predominantly Hyperactive-Impulsive Subtype.
This subtype is diagnosed if there are symptoms of hyperactivity-impulsivity along with fewer symptoms of inattention.
Hyperactivity symptoms
Symptoms include frequent fidgetiness with hands and/or feet or squirming when required to sit still. This child is likely to have difficulty playing or engaging in activities quietly. They may be constantly on the go or talk excessively. Often this child gets up from their seat in class or in other situations where remaining seated is expected. They may run and climb at inappropriate times. As they move into adolescence and adulthood, these ‘active’ behaviours often subside, but their restlessness remains.
Impulsivity symptoms
The impulsive child blurts out answers before the question has been finished and has difficulty waiting their turn. Consequently, they interrupt and disrupt games and conversations.
3. ADHD, Combined Subtype.
This subtype is when the symptoms of both inattention and hyperactivity-impulsivity co-occur.
Caution. Because we all show some of these behaviours across the lifetime, the DSM-V contains specific guidelines for determining whether ADHD is present. The behaviours must appear early in life, before age 7, and continue for at least 6 months. The behaviours must be more frequent and/or severe than others of the same age. The behaviours must cause significant functional impairment in at least two areas of the person’s life (school, work, home or social life).
Other Disorders that can be Co-morbid with (Accompany) ADHD?
One of the difficulties in diagnosing ADHD with a single questionnaire is that ADHD is often co-morbid. QEEG, which examines brain function, can differentiate between disorders which have behavioural overlap. The following are a few examples:
1. Learning Difficulties:
Many children with ADHD also have a specific learning disability (LD), which means that they have trouble mastering language or certain academic skills (e.g., reading, writing or maths). ADHD is not in itself a learning disability. However, because it can interfere with concentration and attention, ADHD can make it just as hard to achieve at school as a learning disability.
Learning disabilities are diagnosed when the person’s achievement on individually administered and standardised tests in reading, mathematics, or written expression is substantially below that of which is expected for their age, schooling, and level of intelligence. Learning disabilities significantly interfere with academic achievement, and/or life skills.
2. PANDAS AND PANS

PANDAS is an acronym for a condition called Paediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcus (PANDAS). Current research suggests that Tourette’s and OCD can, in some cases, result from the effect of the body's own immune system antibodies attacking parts of the brain. PANDAS syndrome onset usually occurs following an Ear, Nose or Throat (ENT) infection from Group A Beta Haemolytic Streptococcus (GABHS). GABHS antibodies can damage parts of the brain resulting in a range of behavioural disorders: OCD, ODD, Tourette’s, ADHD, and psychosis. People with Tourette’s have TICS and other involuntary movements, such as eye blinks, facial twitches, or complex body movements. Others grimace, shrug, sniff, or bark out words. Swearing can also be a manifestation of Tourette’s. Often Tourette’s symptoms are accompanied by symptoms of OCD.
PANS is a more recent name for an autoimmune response to a wide range of organisms that can include bacteria, mycoplasma, or viruses. The symptoms are episodic, meaning that they appear or get worse when there is an infection, such as a sore throat or chest infection. They often settle down until the next episode. Sometimes the brain tissues never completely recover leaving permanent symptoms. PANDAS/PANS is well researched by scientists at the NIH (USA).
Few doctors, paediatricians and psychiatrists understand PANS and PANDAS. As with any new concept, the scientific establishment first refuses to acknowledge it. It may take decades before the concept is widely accepted. For more information, see our PANDAS/PANS WEBPAGE.
3. Oppositional Defiant Disorder and Conduct Disorder

Nearly 50% of children with ADHD have comorbid oppositional defiant disorder (ODD). Children with ODD may overreact or lash out when feeling threatened or challenged. They may be stubborn, have angry outbursts, or act belligerently/defiantly. ODD can worsen, causing serious conduct disorders. Children with ODD are at risk of getting in trouble at school, and with the police. They may take unsafe risks, break laws, steal, set fires, destroy property, and drive recklessly. They must receive help before their early developmental behaviours leads to serious problems.
4. Mood Disorders

Many children with ADHD, predominantly younger children, and girls, have mood disorders. About one-fourth of all children feel anxious. They experience tremendous worry, tension, or uneasiness, even when there is nothing to fear. Because these feelings are scarier, stronger, and more frequent than normal fears, they can affect thought and behaviour. Similarly, depression goes beyond ordinary sadness. Depressed children may feel so down that they feel hopeless and unable to perform tasks. Depression can disrupt sleep, appetite, and the ability to think.
Because mood disorders and attention disorders often go hand in hand, every child with ADHD should be assessed for co-morbid anxiety and depression.
Of course, not all children with ADHD have a co-morbid disorder. Nor do all people with learning disabilities and Tourette’s syndrome, have ADHD. However, when disorders do co-occur, a combination of problems can complicate a person’s life. Comprehensive assessments ensure that all the child’s presenting behaviours are identified.



